Racial Disparities in Severe Maternal Morbidity Linked to Preexisting Health Conditions
UH Study Highlights Need for Improved and Expanded Pre-pregnancy Health Care

Researchers at the University of Houston say Black women in Texas experience severe maternal morbidity nearly twice as often as white women, underscoring a critical need for expanded health care for women well before they are hospitalized for the delivery of their child.
The study from UH’s Institute for Research on Women, Gender and Sexuality finds that preexisting health conditions account for nearly 80% of the Black-white SMM gap, while the remainder could be explained by differences in severity, differences in treatment within the same hospital or from the same physician due to biases, among other factors.
“By a large margin, the major contributor to the Black-white severe maternal morbidity gap is the difference in the comorbidity score between non-Hispanic Black and non-Hispanic white women.”
“Black women exhibit a higher number and different composition of preexistent health conditions, compared to white women upon entering the hospital for delivery,” said Annamaria Milazzo, research assistant professor at the IRWGS. “The data suggest that a vast portion of the disparity can be explained by differences in health status prior to delivery, and it does not seem to be the result of Black women being more likely to use worse hospitals and/or see worse doctors compared to white women."
Where maternal mortality involves a woman’s death due to pregnancy-related causes, SMM cases can be considered near misses for maternal death because they can lead to death if not properly identified and managed.
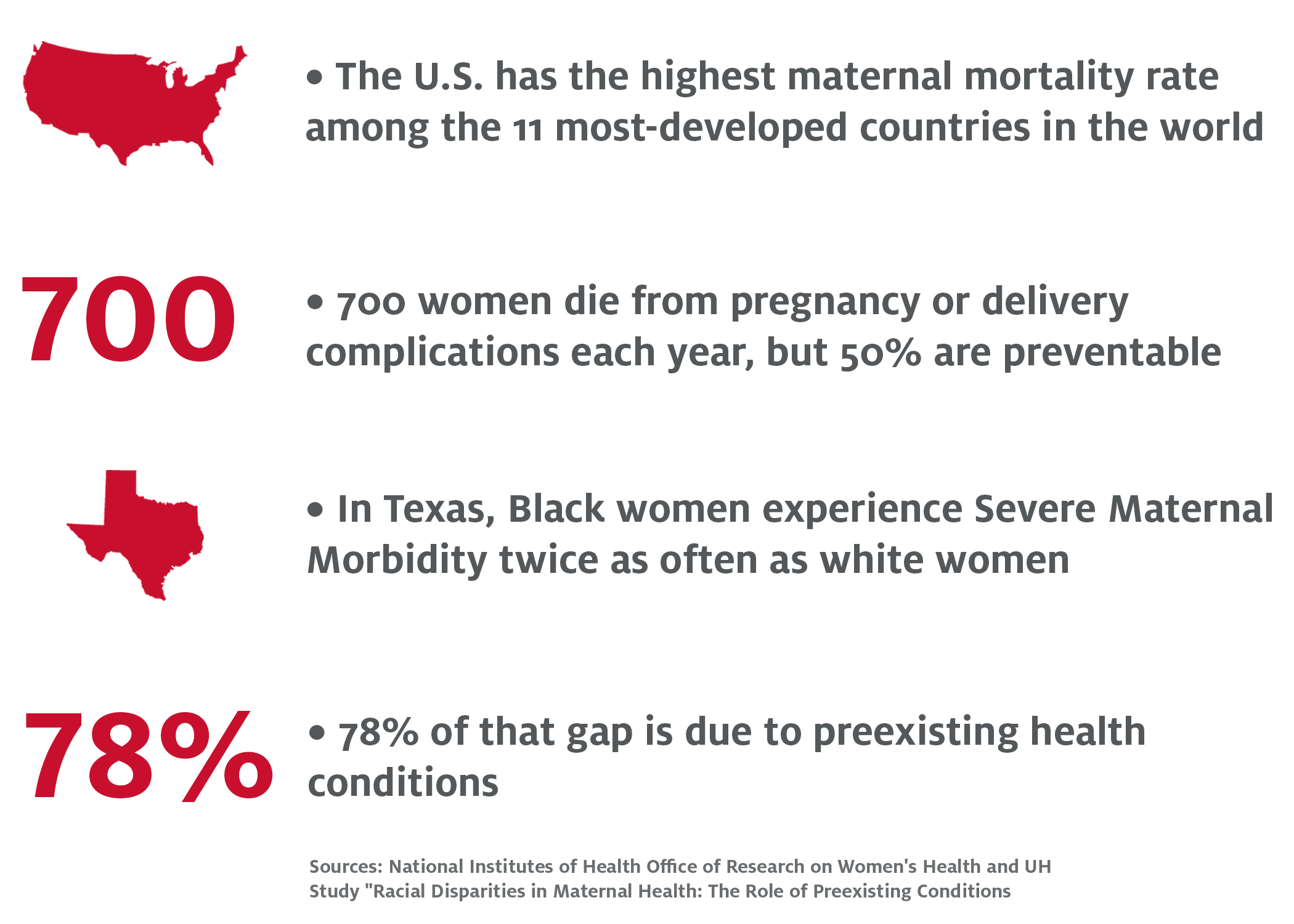
According to the National Institutes of Health’s Office of Research on Women’s Health, the U.S. has one of the highest maternal mortality rates in the developed world with approximately 700 women dying each year because of pregnancy-related causes. Rates of SMM are much higher, with roughly 75 women experiencing it per every maternal death. Black women experience substantially higher rates of both maternal mortality and SMM.
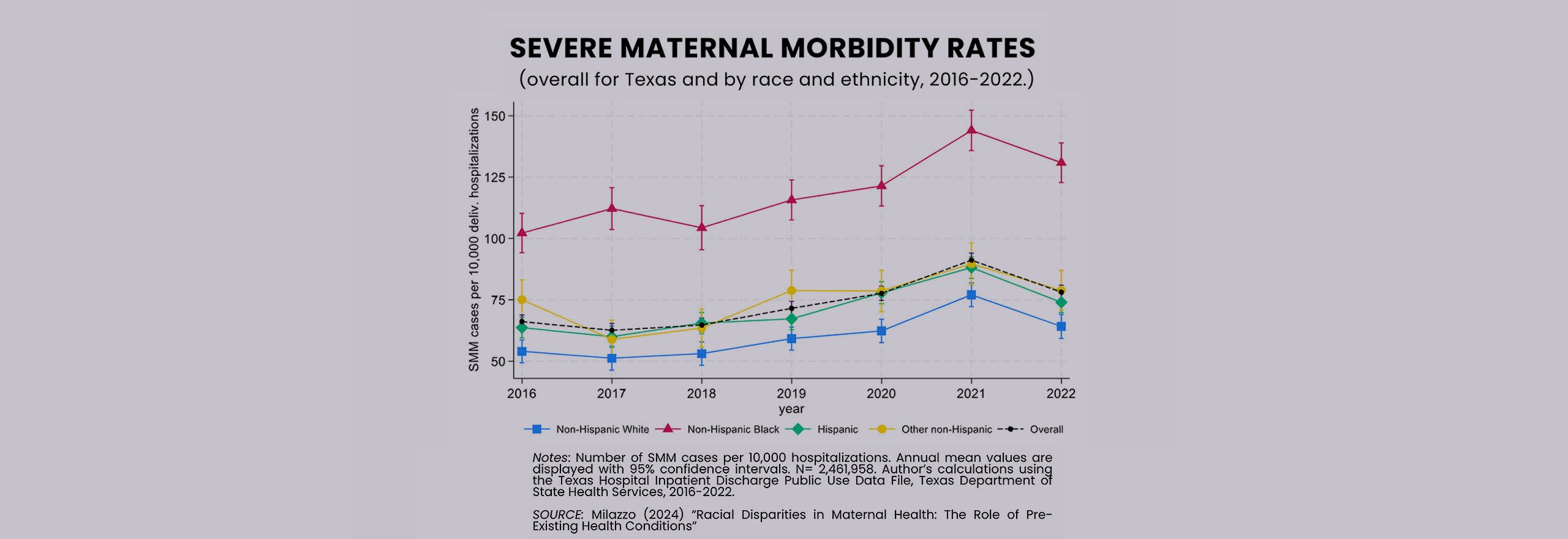
Milazzo looked at hospital inpatient discharge data from all deliveries in Texas from 2016 to 2022 to identify trends and factors in the SMM racial disparity and found a clear need for more focus on women’s health well before they conceive, which could include expanded access to Medicaid. In Texas, with the highest share of uninsured women in the nation, almost 1 in 4 women of reproductive age do not have health insurance. The state is 1 of 10 where Medicaid only becomes available to many low-income women after they become pregnant.
“Better access to comprehensive care pre-conception, including regular check-ups for improved management of medical conditions as they emerge, as well as improved access to prenatal care, could help address these issues,” Milazzo said.
“Overall, the findings underscore the critical need for prioritizing women’s health well before childbirth hospitalization.”
The Institute for Research on Women, Gender and Sexuality is hosting a webinar on Monday, July 8, to present the report’s findings and discuss potential solutions:
What: Webinar on the UH IRWGS Maternal Morbidity Report
When: Monday, July 8, 11 a.m. – 12 p.m.
Click here to register for the webinar.

